The doctors thought they had the malignant cell transformation under control, and Sandra and her boyfriend were planning to have a baby. Then came the letter about relapse. Shortly thereafter, Sandra no longer had a uterus. “They have removed what made me into a woman,” she states. Sandra was twenty-four years old, and although her boyfriend says that biological children isn’t that important to him, it was very important to her.
“Uterus removal – hysterectomy – is the most common gynaecological surgical procedure in Norway. Nevertheless, there are hardly any studies concerning women’s experiences related to this, particularly young women’s experiences,” says Kari Nyheim Solbrække, Associate Professor at the Institute of Health and Society at the Faculty of Medicine, the University of Oslo.
For those who have to remove the ovaries as well, the hysterectomy involves being thrown into menopause. If the uterus is removed due to cancer, you may add the side effects from radiotherapy. The vaginal walls become clogged unless you actively keep them open by the use of a rod.
“Today, women’s health primarily revolves around breast cancer. Breast cancer research is also considered more prestigious. And of course this type of research is important, but it overshadows gynaecological diseases,” claims Solbrække.
Gynaecological cancer as taboo
Solbrække and her colleague Hilde Bondevik have interviewed eight women between the age of twenty-five and forty-three who have gone through hysterectomy. It was extremely difficult to find young women who were willing to participate.
Even some of the members of the Norwegian Gynaecological Cancer Association (‘Gynkreftforeningen’) don’t want to receive their membership journal in the mail. They don’t want anyone to know that they’ve had gynaecologic cancer and removed their uterus, Solbrække notes.
Initially, their plan was to study women’s experiences with hysterectomy more generally, but the researchers ended up with a selection of six women who have had gynaecologic cancer, and just two women who have gone through hysterectomy due to heavy uterine bleeding.
“The study doesn’t say anything in general about the reactions to hysterectomy; rather, it is an in-depth study of young women who have had their uterus removed as a result of gynaecologic cancer and how they experience hysterectomy.”
Common procedure
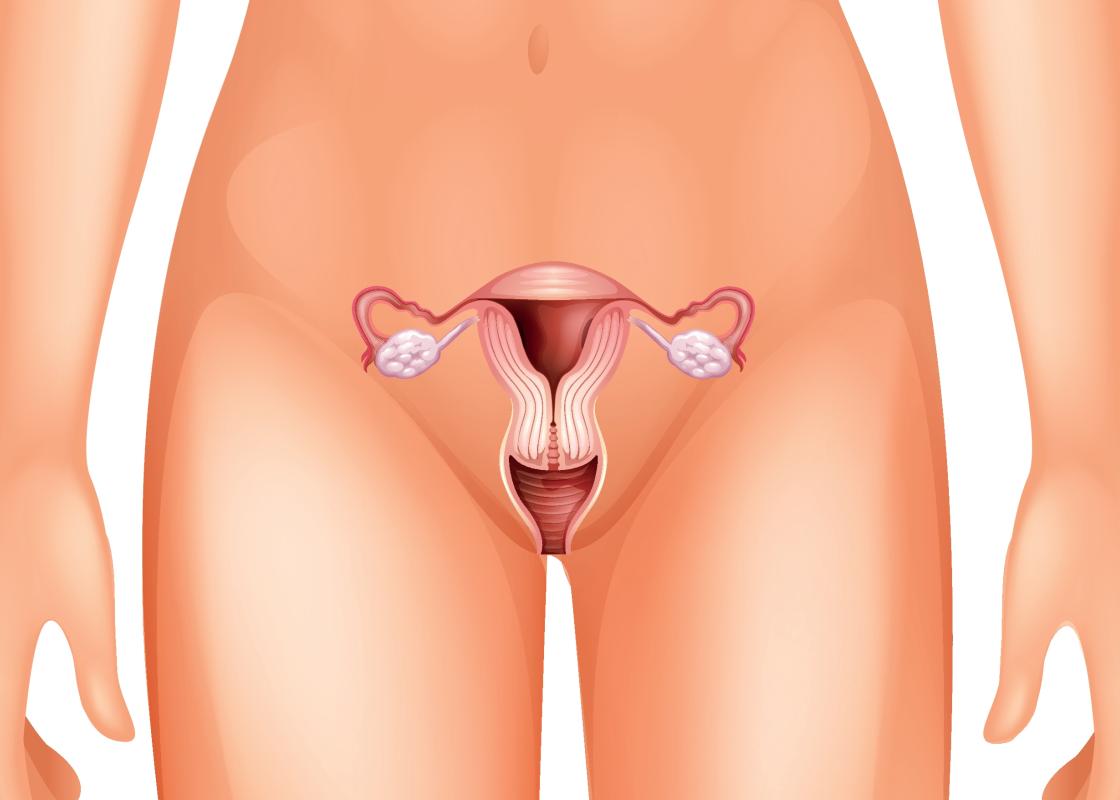
Hysterectomy involves the removal of the uterus, either abdominal (through abdominal incision) or vaginal (through the vagina). Every year more than 5000 women have their uterus removed, mostly due to heavy uterine bleeding, leiomyoma, and pains.
Hysterectomy may be total or partial; some only remove their uterus while others also have one or both of their ovaries, the uterine tubes, the cervix, and surrounding tissues removed.
Approximately 1700 women are diagnosed with gynaecologic cancer every year, around twenty per cent of them of fertile age. Many of these women have to go through uterus removal in order to survive.
The strong desire for biological children
For the six women who are no longer fertile, that is what is most traumatic for them. Sandra feels that life has lost its meaning:
For me the meaning of life was to become a mother, to experience childbirth, and the feelings a couple share while going through pregnancy and birth together. (…) I am so grateful that I have a boyfriend; otherwise, I probably would have ended up alone. I can’t provide men with a child. This definitely makes me less of a woman for them.
“We were a bit surprised to find that this was so existential for these young women in their twenties,” says Solbrække.
“It shows the connection between our physical body and our identity and the significance of this connection even in modern times.”
“You mean the fact that our body’s limits and possibilities are significant for how we define ourselves? Why do you find this surprising?”
“Gender researchers have been concerned with revealing apparently self-evident connections between body and identity. The fact that a woman has a uterus shouldn’t define who we are or which rights we are entitled to. But body and culture is closely linked,” says Solbrække.
“What really struck us was the intense grief related to not being able to become a biological mother. It is easy to think that the younger generation of women will consider other ways of having children as a natural option. It should also be noted that none of our interviewees were newly operated, a few years had passed. Therefore, one would easily expect them to have found alternative ways of becoming parents.”

Reluctant researchers
According to Solbrække, the connection between the physical body and identity related to gender has been a delicate issue within the field of gender research.
“But we have to dare to talk about women’s health. It doesn’t necessarily make us gender essentialists.”
According to her, women’s strong desire to have biological children must be taken seriously and inability should be equated to involuntary childlessness.
“We mustn’t underestimate life projects involving the female body. It is not a human right to have children, but we must take seriously that it still is a common desire for women to have children.”
“It doesn’t help telling them “stop thinking that you want children”, “you may have a good life without children”, or “having children is not everything for a woman”. I think there may be some anxiety related to these issues among gender researchers within certain circles.”
See also: When sex becomes impossible due to burning pain in and around the vulva
Hysterical women governed by their uterus
Perhaps this anxiety is grounded in history.
Etymologically, the term hysterectomy comes from the Greek term hystera, which means uterus.
“Historically, women’s psyche has been linked to the uterus,” says Solbrække.
The term hysterical also originates from hystera, which was regarded as a condition of uncontrollable and exaggerated emotions. During the nineteenth century, hysterectomies were performed grounded in theories that female nervousness was related to a uterus disease. According to the medical expertise of the time, women’s psyche was governed by the uterus and the ovaries. The removal of the uterus was supposed to bring the nerves under control.
“The health personnel today hardly believe that our psyche is governed by the uterus, but perhaps the idea that losing the uterus makes women incomplete and unhappy still exists,” says Solbrække.
It is, however, the sudden end to the dream of becoming a biological parent that bothers the young women in Solbrække’s study. Older women who have their uterus removed due to heavy bleedings are often happy with their lives without a uterus.
Young woman in an old body
Uterus removal due to cancer revolves around more than just losing the opportunity to have biological children. Some women also have to have their ovaries removed. As a result, the women may be thrown into menopause while they’re still in their twenties.
“Many of the women use strong words about their own body, that their body resembles that of an old woman and that they have heavy hair growth. That they never want to go to the beach again,” says Solbrække.
“From being young adults with their life ahead of them, they suddenly find their bodies changing rapidly. It is hard to accept, and it is difficult to talk to others about it. We don’t possess the right language.”
The women feel that they don’t get enough information about life after surgery. According to the researcher, this is under communicated both in society in general and within the cancer rehabilitation programs that they take part in.
Clogged vaginal walls
The side effects to the cancer treatment itself come on top of everything. Some experience major problems with their own sexuality, not only because of menopause, but also because their vaginal walls become clogged as a result of radiotherapy.
According to a Norwegian study of men with prostate cancer, the men found that the health personnel talked too much about impotence, while the men themselves were more concerned with the fact that they had been diagnosed with cancer. In comparison, the women with gynaecologic cancer experience that their sexuality after treatment is not an issue, notes the researcher.
The women are given a rod to bring home in order to keep their vulva open. This is, however, not what these women focus on in the middle of a life crisis.
“Several of the women have told me that they are only given a box with a rod and told to use it when they get home. This rod often ends up in a drawer, as these women are in a completely different place mentally. When they pick it up two months later things have already started happening down there,” says Solbrække.
“It says something about the lack of gravity and professionalism related to this type of treatment. Several of the women feel that they weren’t properly looked after, and they feel that this neglect is directly related to their diagnosis.”
Diagnosis with sexual connotations
Gynaecologic cancer is associated with the HPV virus, which is sexually transmittable. Several of Solbrække and Bondevik’s interviewees were asked how many sex partners they’d had by the health personnel, and they’ve experienced a lot of stigma related to gynaecologic cancer. They think this might be one of the reasons why they are treated poorly.
“Whether or not it is true that this is related to their diagnosis and whether they are more neglected than other patients is impossible to measure. What is significant here is that this is how they experience it,” says the researcher.
“Why is that important?”
“Equal health services is a Norwegian ideal. Therefore, we tend to believe strongly in good, knowledge-based treatment of all diagnoses. It is unacceptable that some people feel like second-rate cancer patients.”
Breast cancer is the golden standard
“Cancer is one of our most widespread diseases. More and more people survive the disease due to continuous medical improvements. In Norway, we have more than two hundred thousand survivors of cancer today. Many of them are doing well, but many also experience complications. These complications are under communicated in society.”
“Within critical cancer research, it is a common opinion that the survivors of breast cancer have set the golden standard for how a survivor of cancer is supposed to behave,” says Solbrække.
“Researchers call it ‘breast-cancerisation’. According to this golden standard, cancer survivors are supposed to be positive and heroic. They’re supposed to come out of treatment as stronger human beings, as happy survivors.”
There exist carefully developed preliminary and follow-up treatments for women who are diagnosed with breast cancer, and the whole world is conscious about their disease. Celebrities have come forward, people bake breast-shaped cup cakes and sell pink ribbons for fundraising, and numerous stories about the disease are being written, filmed, and photographed.
“Many international studies on gynaecologic cancer show that some of the affected women go through treatment almost without knowing what type of cancer they have or what kind of treatment they are receiving,” says Solbrække.
“We’ve yet to see a celebrity come forward to say she’s been treated for gynaecologic cancer, as one of our interviewees remarked.”
See also: "Heart disease is the number one killer of women in Norway"
Translated by Cathinka Dahl Hambro
- Kari Nyheim Solbrække and Hilde Bondevik are both Associate Professors at the Institute of Health and Society at the Faculty of Medicine, the University of Oslo.
- Their article Absent Organs - Present selves: Exploring embodiment and gender identity in young Norwegian women's accounts of hysterectomy was recently published in International Journal of Qualitative Studies on Health and Well-being.
- The research is based on in-depth interviews with eight women who have undergone hysterectomy, six of which were treated for gynaecologic cancer.
- Other publications based on the same material are in progress.
- Solbrække and Bondevik are also working on other projects related to their research on life with gynaecologic cancer, and the effect of prestige related to the research and treatment of certain types of cancer.